Do greenspace and main road exposure affect mental wellbeing?
Originally submitted: April 2022
While the answer may seem pretty intuitive, carrying out an experiment to prove or disprove my hypotheses taught me that things are rarely as straightforward as they seem, and that when it comes to experimental design there is always room for improvement. This whole-course project was a lot of fun to work on despite the challenges that Covid threw at us.
Introduction
Place is widely acknowledged as a contributing factor to wellbeing. For example, the effects of exposure to greenspace and main roads/traffic on physical health are well-researched. Claimed greenspace effects are widely positive, including increased physical activity in children and reduced type two diabetes and obesity risk (Almanza et al., 2012; De la Fuente et al., 2020); meanwhile for main roads/traffic they are generally negative, including increased risk of atopic diseases and allergic sensitisation in children (Morgenstern et al., 2008). However, this report will focus on both greenspace and main road exposure and their relationship with mental wellbeing.
Exposure studies such as those mentioned approach measurement in various ways falling under the categories of static and dynamic. Static exposure only measures exposure from fixed locations, usually based on participants’ home addresses. This makes it easy to obtain exposure data, especially if it is already accessible from another source; however it assumes participants always remain at home. Adding buffers can help, but that assumes people only go to the places closest to them. Most importantly, static exposure fails to consider how people travel between places.
Dynamic exposure can take account of travel routes and therefore may be preferable, as it assigns exposure more accurately across space-time. While constantly tracking someone’s location may have seemed too difficult two decades ago, the answer now lies in our pockets: smartphones can record the necessary data in a relatively simple and unobtrusive way. As Harari et al. (2016, p. 839) put it, smartphones capture our “mobility behaviors (where we are via accelerometer, global positioning system [GPS], and WiFi) as part of their daily functioning”, and therefore appear to be an ideal way for health geographers to carry out exposure research - all this data can be collected without the need for special equipment, participant interviews or diaries, thus increasing cost- and time-efficiency, and of course, accuracy.
Methods
To measure mental wellbeing we used the 14-item Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS), which was “developed to enable the measuring of mental wellbeing in the general population and the evaluation of projects, programmes and policies which aim to improve mental wellbeing” (Stewart-Brown, n.d.). Each of the items is scored from one to five, giving a range of 14 to 70, where a higher score suggests better mental wellbeing.
To measure dynamic exposure to greenspace and main roads, we collected smartphone location data using the app FollowMee. Participants kept back-up diaries, noting the time they spent at and away from home, the locations they visited, and other aspects that would assist with writing this report. The location data was then compared to 100-metre buffers around greenspace and main roads within the study area (Christchurch), and exposure to each (as the percentage of data points within the buffer) was calculated using the GIS software ArcMap. The greenspace, main roads and study area were supplied to us as pre-prepared layers. We measured static exposure to the two variables using participants’ home addresses, which were exposed or not exposed depending on whether they were located within the buffers.
Further data analysis was carried out using Microsoft Excel and R/RStudio.
Hypotheses
I expect there will be a positive relationship between exposure (both static and dynamic) to greenspace and mental wellbeing. It is widely accepted that being out in nature (or even just seeing it) can lift one’s mood; this is supported by studies such as Beyer et al. (2014) and Jiang (2022). I imagine static exposure to greenspace will increase dynamic exposure to greenspace, as having greenspace on your doorstep may act as motivation to utilise it more often, as suggested by studies like Nielsen and Hansen (2007).
Conversely, I expect there will be a negative relationship between static and dynamic exposure to main roads and mental wellbeing. I think static exposure will have a stronger impact because of the stress of not being able to avoid associated noise or fumes in your own home, which is supported by studies like Jensen et al. (2018) and Shepherd et al. (2016). For dynamic exposure I expect the impact on mental wellbeing will be less salient, however those with the highest dynamic exposure may be noticeably impacted because this implies they may spend more time driving, which increases negative health outcomes (Ding et al., 2014). I think static exposure will not discernibly impact dynamic exposure, as whether you live near main roads does not change the fact that we all need to use them to access most places.
Results
Our sample was 65 [course name redacted] students at the University of Canterbury. It is important to note these students were also responsible for carrying out this study.
| Exposed | Not exposed | |||
|---|---|---|---|---|
| Count | Percentage | Count | Percentage | |
| Static greenspace exposure | 21 | 32.31 | 44 | 67.69 |
| Static main road exposure | 24 | 36.92 | 41 | 63.08 |
Figure 1: Counts and percentages of individuals whose residence (static exposure site) was/was not exposed to greenspace or main roads.
| Exposed | Not exposed | |
|---|---|---|
| Mean WEMWBS wellbeing score | ||
| Static greenspace exposure | 49.95 | 48.52 |
| Static main road exposure | 46.75 | 50.29 |
Figure 2: Mean WEMWBS wellbeing scores split by whether individuals were/were not statically exposed to greenspace or main roads.
| Mean (average) | Standard deviation | |
|---|---|---|
| Dynamic greenspace exposure | 22.46 | 19.11 |
| Dynamic main road exposure | 33.72 | 22.31 |
| WEMWBS wellbeing score | 48.98 | 7.38 |
Figure 3: Mean and standard deviation values for the sample group’s dynamic greenspace and main road exposure percentages and their WEMWBS wellbeing scores.
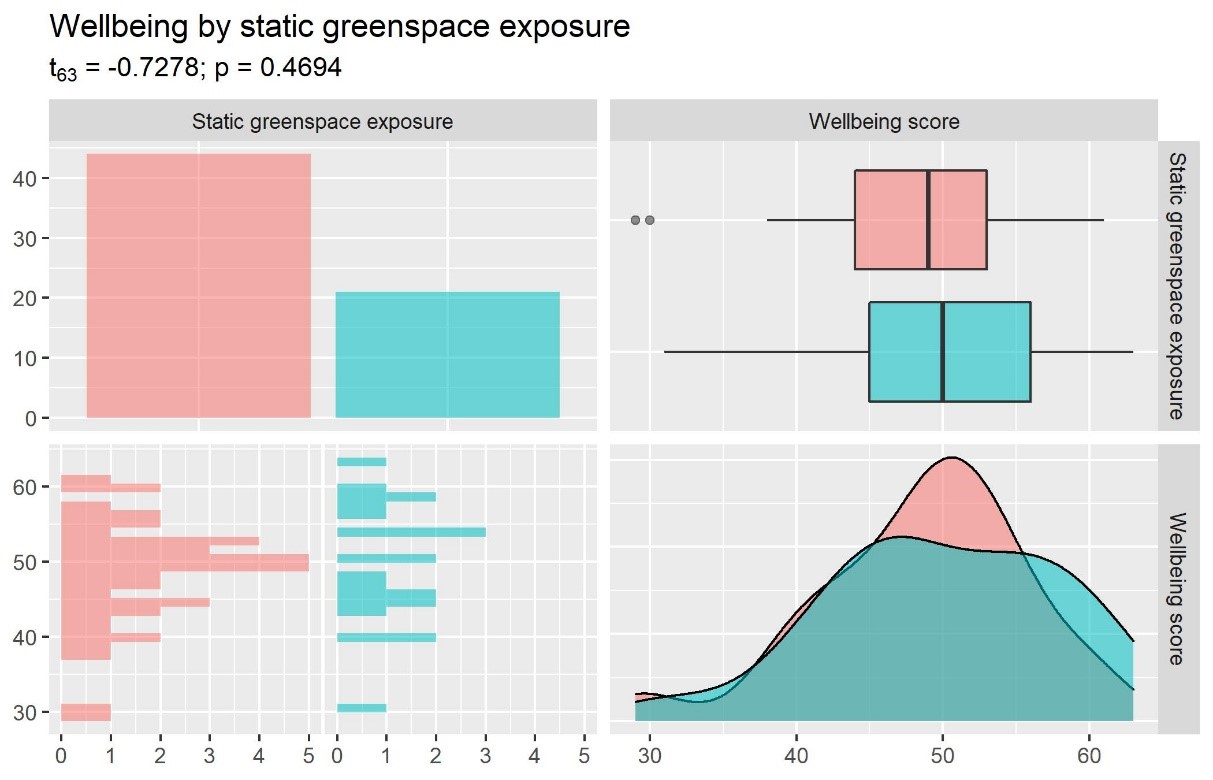
Figure 4: Bar plot, box plot, histogram and density plot showing the relationship between static greenspace exposure and wellbeing score. Red = not exposed, blue = exposed.
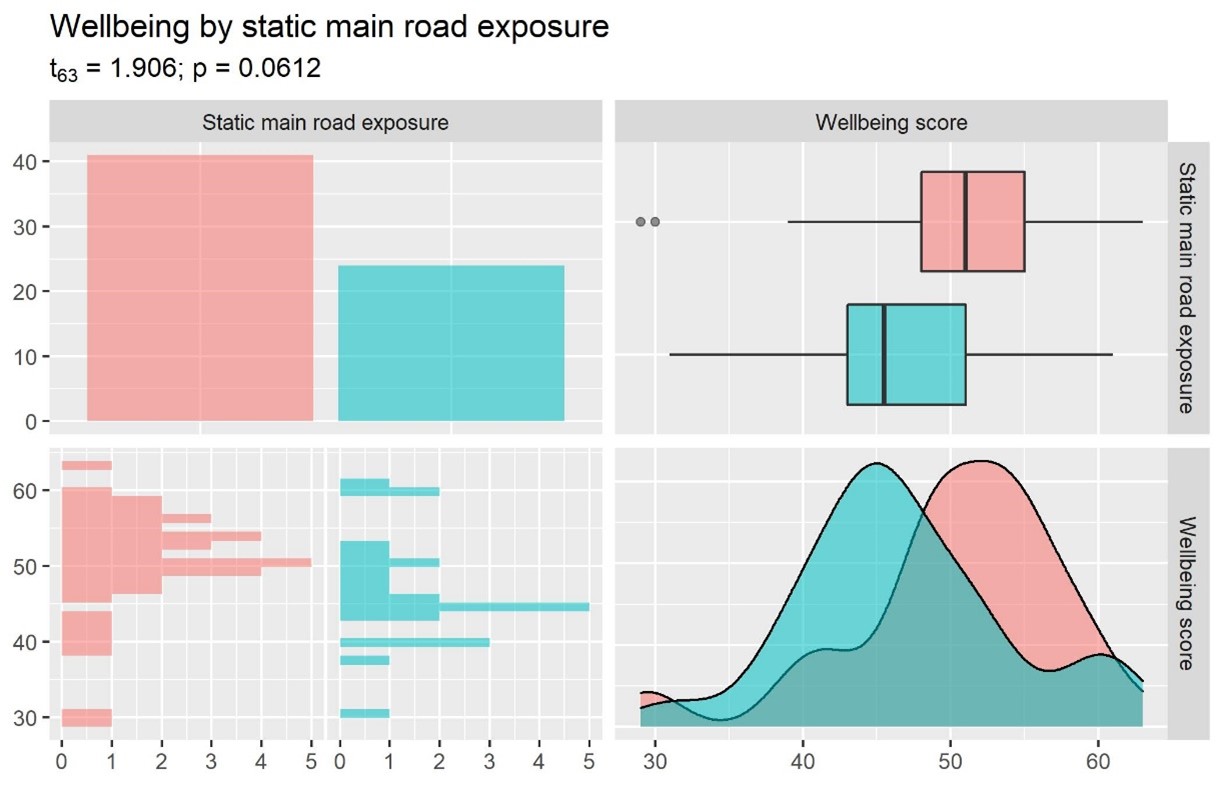
Figure 5: Bar plot, box plot, histogram and density plot showing the relationship between static main road exposure and wellbeing score. Red = not exposed, blue = exposed.
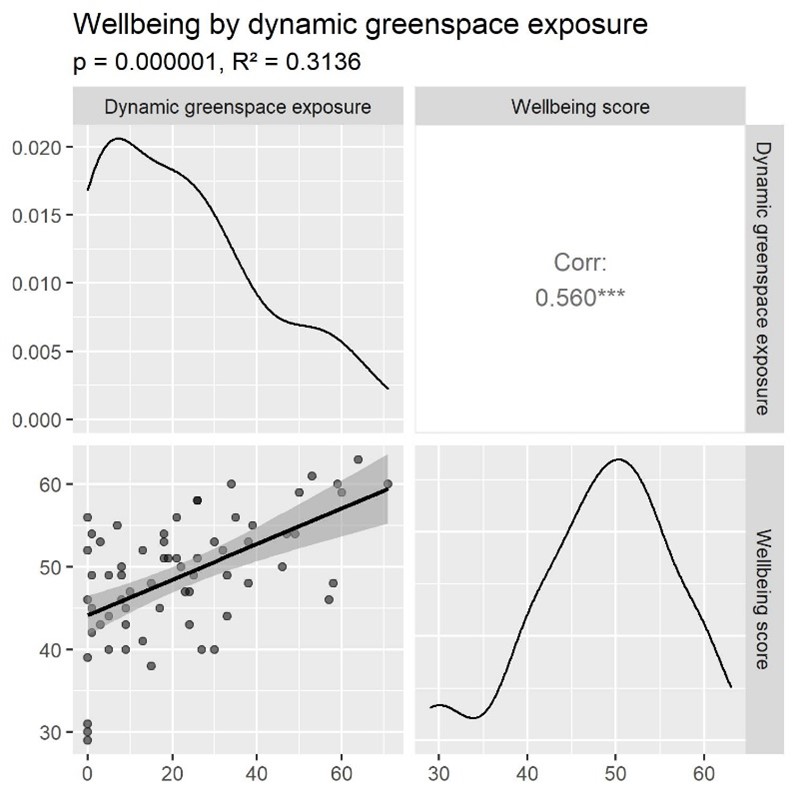
Figure 6: Density plots, correlation and scatter plot showing the relationship between dynamic greenspace exposure and wellbeing score.
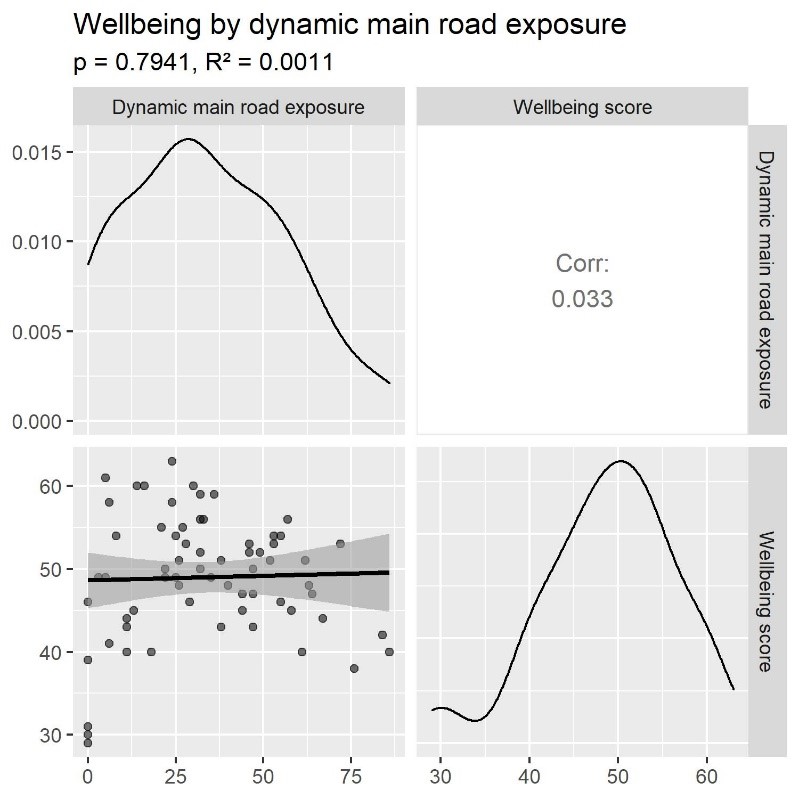
Figure 7: Density plots, correlation and scatter plot showing the relationship between dynamic main road exposure and wellbeing score.
Wellbeing by static greenspace exposure
Figure 1 shows a majority of the sample (67.69%) was not exposed to greenspace at their residence. The mean wellbeing score of those exposed is 49.95, while the mean score of those not exposed is 48.52, as shown in Figure 2. For reference, the overall mean wellbeing score (Figure 3) is 48.98, with a standard deviation of 7.38. As illustrated by the box plot in Figure 4, there are two potential outliers who were not exposed and scored around 30. While the mean wellbeing score of those who were statically exposed to greenspace is higher than that of those who were not, the difference is not great enough for the relationship to be statistically significant, as evidenced by the p-value of 0.4694.
Wellbeing by static main road exposure
Figure 1 shows a majority of the sample (63.08%) was not exposed to main roads at their residence. The mean wellbeing score of those exposed is 46.75, while the mean score of those not exposed is 50.29, as shown in Figure 2. As seen in the box plot in Figure 5, there are two potential outliers who were not exposed and scored around 30. The curves of the two groups in the density plot in Figure 5 are much more separate than those in Figure 4. The curve of those who were not exposed is right skewed, while the other curve is closer to having no skew. Regardless, the relationship is not statistically significant, as proven by the p-value of 0.0612.
Wellbeing by dynamic greenspace exposure
The correlation coefficient of 0.560 (Figure 6) means there is a strong positive relationship (Cohen, 1992); this can be seen in the scatterplot’s trendline. The scatterplot also shows three potential outliers with a dynamic exposure of 0 and a wellbeing score around 30. The R2 of 0.3136 means 31.36% of the sample fits the regression model. This relationship is statistically significant, as shown by the p-value of 0.000001.
Wellbeing by dynamic main road exposure
The correlation coefficient of 0.033 (Figure 7) means there is a weak positive relationship (Cohen, 1992); this can be seen in the scatterplot’s trendline. The scatterplot also shows three potential outliers with a dynamic exposure of 0 and a wellbeing score around 30. The R2 of 0.0011 means 0.11% of the sample fits the regression model. This relationship is not statistically significant, as shown by the p-value of 0.7941.
Overall observations
It seems static and dynamic exposure influence mental wellbeing differently, as their results differ in strength, direction, and/or significance. For example, the relationship between wellbeing and dynamic greenspace exposure was a statistically significant strong positive, yet any relationship between wellbeing and static greenspace exposure was slight and insignificant.
These results are somewhat different from my hypotheses. Aside from the relationship between wellbeing and dynamic greenspace exposure, my other hypotheses were disproven due to any relationship being insignificant, although the relationship between wellbeing and static main road exposure was close to being significant. The most surprising result was the (statistically insignificant) weak positive relationship between wellbeing and dynamic main road exposure; while I did not expect the correlation to be strong due to the common necessity of using main roads, I did not think it would be positive.
Discussion
The results suggest dynamic greenspace exposure has a strong positive relationship with wellbeing – the sole exposure variable of our study to have a significant relationship. This implies mental wellbeing is improved by spending more time exposed to greenspace.
Compared to my hypotheses and previous research this makes sense, because other studies have found greenspace exposure can positively affect other health aspects, however we did not find the expected results for the other relationships. These outcomes could be influenced by various confounding factors and limitations which I will discuss.
Confounding factors
Beginning with COVID-19, it is fair to assume associated restrictions and caution have impacted people’s degree of mobility – not just for those participants stuck in isolation during the tracking week, but even for those who could move freely but perhaps chose to limit their movements to lower their risk of catching the virus (Warren and Skillman, 2020).
Transport modes could affect how exposed people feel to greenspace and main roads. Take walking versus driving past a park, where the walker may feel more connected to the greenspace; or cycling on a main road compared to being in a bus, where the cyclist may feel more exposed to air pollution and potential accidents (Zuurbier et al., 2010).
Awareness of the study and tracking could affect where and how often people choose to move due to the Hawthorne effect (Campbell et al., 2021). Personally, I felt motivated to get out and about to make my data more ‘interesting’, otherwise I would have stayed at home as much as possible because of COVID-19 caution; similarly people could avoid going to places they normally would because of a perceived lack of privacy.
While it may be true that exposure to greenspace positively affects wellbeing, this effect could change according to factors such as time of day and perceived attractiveness and safety of the greenspace; for example, a pleasant walk through the park can instead be stressful if undertaken at night (Gatrell et al., 2011).
Motivation for accessing greenspace is an important confounding factor that could be at play in our one significant relationship. Smith et al. refer to this as selective daily mobility bias, in which “an individual’s preference to perform an activity may bias any associations observed” (2019, p. 2). In our case, participants with better mental wellbeing may simply choose to be in/around greenspace more often.
Accuracy
In my opinion the tracking app, FollowMee, left the potential for plenty of errors. Leaving participants in charge of regularly downloading their data meant that data could be omitted due to forgetfulness, and if not set up correctly the app would not constantly record location data. This happened to me, however I managed to retrieve my Google location data and edit it down to the required time and format in R; for participants without such knowledge (especially if participants were not the same people running the study), it is questionable whether such errors could be avoided or picked up on. Some participants clearly falsely recorded their dynamic exposure as 0, because they are also marked as exposed to the corresponding static variable (it is possible, but less likely, that they got the static exposure wrong).
As for issues with GPS accuracy, when looking at my data in ArcMap I noticed my location was recorded in places I had not been; these datapoints had an unusually high ‘accuracy’ assigned to them (representative of poor position dilution of precision, I assume). Other positioning errors that can affect GPS accuracy include multipath (signals bounce off surfaces), obstruction (signals are blocked) and atmospheric (signals are refracted and slowed down).
While the WEMWBS is comparatively intuitive, there is still room for misunderstandings. The score is meant to reflect participants’ general state of mental wellbeing, however when answering it can be easy for participants to be influenced by their current mood. While one could assume the three potential outliers pointed out earlier have such low wellbeing scores because they were just unhappy at the time of scoring, that cannot be proved without further investigation.
The greenspace and main roads layers provided to us for use in ArcMap were of unknown origin and date. If they were created by an unreliable source or not maintained to reflect changing roads and land use, subsequent data generated from them could be inaccurate.
This all means our results are susceptible to various accuracy issues, which should be taken into mind when interpreting them. Most importantly, while dynamic exposure paints a much more accurate picture than static exposure, we must accept it is still not a perfect reflection of dose.
Other limitations
Only tracking participants for a week means we potentially missed variation, as people are unlikely to visit all the usual places within their activity space in that timeframe. For example, I tend to go to a different supermarket every other week, but that was not captured in my tracking data.
When measuring exposure and wellbeing consecutively, we are assuming there is no latency in the relationship. This discounts the possibility that wellbeing could be improved by dynamic greenspace exposure that occurred two weeks ago, for example. This relates to the last point, as longer tracking periods may help to identify latency (Briggs, 2001).
Since the same people carrying out this study participated in it, we knew what results we wanted and could have manipulated our data accordingly. Aside from that source of bias, it is important to consider possible inequalities between individuals, groups and places which were not reflected proportionally in our sample. All participants were students, whose activity spaces (and therefore exposures) are likely to differ considerably from non-students, as “the spatial structure of activity space largely depends on the socioeconomic characteristics of individuals, the environment settings, and the way in which space is perceived” (Ren, 2016). These differences mean our sample cannot be said to represent the wider population.
Buffers, although a simple concept, can be problematic. By using 100-metre buffers, we are assuming everyone at every point within that buffer is exposed. In doing so we invoke the uncertain geographic context problem, because we are not truly certain of “the relevant spatiotemporal contexts in which an individual is exposed to environmental influences” (Kwan, 2012; cited in Park and Kwan, 2017, p. 86). Put another way, while someone walking alongside a park may be exposed to its benefits, someone else around the corner may not even notice the park, yet they are both considered ‘exposed’. This also relates to the ecological fallacy, because deciding that everyone within the buffer is exposed glosses over the fact that they can all be exposed (or not exposed) to different degrees. We could try to fix this by reducing the buffer’s size or changing its shape to reflect something like road networks, but these ‘fixes’ just reflect the two modifiable areal unit problem effects: scale and zoning.
Alternative approaches and further research
Some scholars fear that qualitative humanities skills are giving way to “superficial number crunching” (DeLyser and Sui, 2013, p. 295). When taking quantitative approaches to evaluating exposure and wellbeing it could be argued we are missing balance and context; therefore perhaps a mixed-methods approach would be better.
Some common ways of integrating qualitative elements in health geography include surveying participants (Chaix et al., 2013), and conducting go-alongs or follow-up interviews (DeLyser and Sui, 2013). However, these methods can be quite time- and resource-intensive. The ideal option could be ecological-momentary assessment (EMA), where participants’ phone location data is used to notify them with questions depending on where they are (Pejovic et al., 2015; cited in Harari et al., 2016).
Failing qualitative data acquisition, more context could be gleaned from a tool we are already using: the smartphone. Capturing behavioural-inference data instead of just raw-sensor data could help us “to make inferences about the participant’s behavior” (Harari et al., 2016, p. 846).
It is important to also consider other health measures. Another test may prove more accurate for measuring mental wellbeing, for example the General Health Questionnaire (GHQ), with its different phrasing and more complex scoring system. Alternatively, if we used the EMA approach, we could create custom questions that the participant is requested to answer when they come within exposure range. As an entire questionnaire may be too long to answer so frequently, our questions would be fewer but tailored to the influences on mental health we expect to see (for example, ‘do you feel calm?’) and there would be a minimum delay between notifications.
My suggestion for a re-run of this study is to use the EMA approach with custom questions as mentioned above, paired with behavioural-inference data (captured by Google instead of FollowMee) which is cleaned to remove datapoints above a certain ‘accuracy’ value. This study would run for at least a month, and would ideally have a larger, more representative sample, as this would improve the degree to which our findings reflect the wider population; though it must be noted that increasing timeframe and sample size will require increased resources and time, and increases the potential number of errors. Further research could focus on identifying and quantifying confounding factors in the relationship between dynamic greenspace exposure and wellbeing.
Privacy and ethics
Any form of tracking must begin with informed consent due to the sensitivity of the data being collected. Participants must understand the nature of the data they are sharing, what it will be used for, and how they can access/withdraw it if necessary. With contributed geographic information (CGI), participants generally forego any control outside of that; this brings up the question of whether health geography should move towards volunteered geographic information (VGI), where participants are actively responsible for data collection, as a more ethical method (Blatt, 2015). However, it is uncertain what the liability and consequences would be for inaccurate VGI, or how it could be verified (Blatt, 2015).
The sensitivity of tracking data presents multiple privacy risks. Unsafe handling/storage of data could breach confidentiality – in our case, an example could be the saving of tracking data to a public drive when using the lab computers. Because this data is so detailed, the owner could be identified and their safety or reputation could be harmed.
Many concerns about tracking stem from its role in today’s surveillance society. Some scholars see it as another form of colonialism, and ask us to consider “whether the knowledge it produces is controlled by a technocratic, elite minority or the broader polities that are subjects of surveillance” (Bashford, 2006 and Weir and Mykhalovskiy 2006; cited in French and Smith, 2013, p. 386). French and Smith warn that health surveillance could aid (intentionally or not) in social control, subjectivity formation, and actuarialism (2013). Along the lines of VGI, this leads others to call for “participatory GIS” or “collective health intelligence” (Gatrell and Elliott, 2014, p. 96).
According to Harari et al., “smartphone-sensing research demands transparency between researchers and participants as a central research practice” (2016, p. 849). It is suggested such transparency could include providing the aims and findings to participants alongside copies of their data (Harari et al., 2016). But without further support or suggestions, the sudden “visibility” of this data and the impulse to draw conclusions may negatively impact participants due to the healthism narrative which ignores “the social and economic determinants of health” and places responsibility for health squarely on the individual (Lupton, 2013, pp. 397, 400).
Conclusion
In summary, this study found that dynamic exposure to greenspace has a strong positive relationship with mental wellbeing, while failing to find sufficient evidence for relationships between wellbeing and dynamic exposure to main roads or static exposure to either variable. This report went on to detail the benefits and accessibility of the dynamic approach along with our methods and results, followed by an in-depth discussion of potential flaws in the study and how it could be improved. While there is much room for improvement, this reflects the developing field of mobile health research.
Based on the results of this study, I recommend the implementation of a policy to oversee the creation/preservation of greenspaces in urban areas, while encouraging their use through a health promotion campaign. This campaign would have two main parts: A media campaign encouraging people to visit their local parks, and an extension of the Green Prescription initiative to cover mental health. The media campaign would be aimed at the general population, whereas the Green Prescription would target those with lower wellbeing, who perhaps lack the motivation to visit greenspaces otherwise. While generally used to prescribe sports or healthy eating programmes to people with physical health issues, prescription of greenspace-based activities such as guided Botanic Gardens walking tours, birdwatching, or even just spending a certain amount of time in greenspace could also improve mental health (Ministry of Health, n.d.).
References
Almanza, E., Jerrett, M., Dunton, G., Seto, E., & Pentz, M. A. (2012). A study of community design, greenness, and physical activity in children using satellite, GPS and accelerometer data. Health & Place, 18, 46-54. https://doi.org/10.1016/j.healthplace.2011.09.003
Beyer, K., Kaltenbach, A., Szabo, A., Bogar, S., Nieto, F., & Malecki, K. (2014). Exposure to neighborhood green space and mental health: Evidence from the survey of the health of Wisconsin. International Journal of Environmental Research and Public Health, 11(3), 3453–3472. http://doi.org/10.3390/ijerph110303453
Blatt, A. J. (2015). Health, science, and place. Springer.
Briggs, D. J. (2001). Exposure assessment. In P. Elliott, J. Wakefield, N. Best, & D. J. Briggs (Eds.), Spatial epidemiology: Methods and applications. Oxford Scholarship Online. https://doi.org/10.1093/acprof:oso/9780198515326.003.0019
Campbell, M., Marek, L., & Hobbs, M. (2021). Reconsidering movement and exposure: Towards a more dynamic health geography. Geography Compass, 15, e12566. https://doi.org/10.1111/gec3.12566
Chaix, B., Méline, J., Duncan, S., Merrien, C., Karusisi, N., Perchoux, C., Lewin, A., Labadi, K., & Kestens, Y. (2013). GPS tracking in neighborhood and health studies: A step forward for environmental exposure assessment, a step backward for causal inference? Health & Place, 21, 46-51. https://doi.org/10.1016/j.healthplace.2013.01.003
Cohen, L. (1992). Power primer. Psychological Bulletin, 112(1), 155-159.
De la Fuente, F., Saldías, M. A., Cubillos, C., Mery, G., Carvajal, D., Bowen, M., & Bertoglia, M. P. (2020). Green space exposure association with type 2 diabetes mellitus, physical activity, and obesity: A systematic review. International Journal of Environmental Research and Public Health, 18(1), 97. http://doi.org/10.3390/ijerph18010097
DeLyser, D., & Sui, D. (2013). Crossing the qualitative-quantitative divide II: Inventive approaches to big data, mobile methods, and rhythmanalysis. Progress in Human Geography, 37(2), 293-305. https://doi.org/10.1177/0309132512444063
Ding, D., Gebel, K., Phongsavan, P., Bauman, A. E., & Merom, D. (2014). Driving: A road to unhealthy lifestyles and poor health outcomes. PLOS ONE, 9(6), e94602. https://doi.org/10.1371/journal.pone.0094602
French, M., & Smith, G. (2013). ‘Health’ surveillance: New modes of monitoring bodies, populations, and polities. Critical Public Health, 23(4), 383-392. https://doi.org/10.1080/09581596.2013.838210
Gatrell, A. C., Elliott, S. J., & Williams, A. (2011). Mobilities and health. Taylor & Francis Group.
Gatrell, A. C., & Elliott, S. J. (2014). Geographies of health: An introduction. John Wiley & Sons, Incorporated.
Harari, G. M., Lane, N. D., Wang, R., Crosier, B. S., Campbell, A. T., & Gosling, S. D. (2016). Using smartphones to collect behavioral data in psychological science: Opportunities, practical considerations, and challenges. Perspectives on Psychological Science, 11(6), 838-854. https://doi.org/10.1177/1745691616650285
Jensen, H. A. R., Rasmussen, B., & Ekholm, O. (2018). Neighbour and traffic noise annoyance: a nationwide study of associated mental health and perceived stress. European Journal of Public Health, 28(6), 1050-1055. https://doi.org/10.1093/eurpub/cky091
Jiang, S. (2022). Nature through a hospital window: The therapeutic benefits of landscape in architectural design. Routledge.
Lupton, D. (2013). Quantifying the body: Monitoring and measuring health in the age of mHealth technologies. Critical Public Health, 23(4), 393-403. https://doi.org/10.1080/09581596.2013.794931
Ministry of Health. (n.d.). How the Green Prescription works. https://www.health.govt.nz/our-work/preventative-health-wellness/physical-activity/green-prescriptions/how-green-prescription-works
Morgenstern, V., Zutavern, A., Cyrys, J., Brocklow, I., Koletzko, S., Krӓmer, U., Behrendt, H., Herbarth, O., von Berg, A., Bauer, C. P., Wichmann, H.-E., & Heinrich, J. (2008). Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. American Journal of Respiratory and Critical Care Medicine, 177(12), 1331-1337. https://doi.org/10.1164/rccm.200701-036oc
Nielsen, T. S., & Hansen, K. B. (2007). Do green areas affect health? Results from a Danish survey on the use of green areas and health indicators. Health & Place, 13, 839-850. https://doi.org/10.1016/j.healthplace.2007.02.001
Park, Y. M., & Kwan, M.-P. (2017). Individual exposure estimates may be erroneous when spatiotemporal variability of air pollution and human mobility are ignored. Health & Place, 43, 85-94. http://doi.org/10.1016/j.healthplace.2016.10.002
Ren, F. (2016). Activity Space. In Oxford Bibliographies Online. Oxford University Press. https://doi.org/10.1093/OBO/9780199874002-0137
Shepherd, D., Dirks, K., Welch, D., McBride, D., & Landon, J. (2016). The covariance between air pollution annoyance and noise annoyance, and its relationship with health-related quality of life. International Journal of Environmental Research and Public Health, 13, 792. https://doi.org/10.3390/ijerph13080792
Smith, L., Foley, L., & Panter, J. (2019). Activity spaces in studies of the environment and physical activity: A review and synthesis of implications for causality. Health & Place, 58, 102113. https://doi.org/10.1016/j.healthplace.2019.04.003
Stewart-Brown, S. (n.d.). The Warwick-Edinburgh Mental Wellbeing Scales – WEMWBS. Warwick Medical School. https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs
Warren, M. S., & Skillman, S. W. (2020). Mobility changes in response to COVID-19. arXiv. https://doi.org/10.48550/arXiv.2003.14228
Zuurbier, M., Hoek, G., Oldenwening, M., Lenters, V., Meliefste, K., van den Hazel, P., & Brunekreef, B. (2010). Commuters’ exposure to particulate matter air pollution is affected by mode of transport, fuel type, and route. Environmental Health Perspectives, 118(6), 783-789. https://doi.org/10.1289/ehp.0901622